Snakebite is a calamity that besets mostly poor, rural populations in some of the least developed nations on earth. In these settings it is but one of a myriad of public health issues facing governments who often have no formal reporting systems for births and deaths, let alone individual illnesses or diseases. Obtaining accurate data on the burden of injury or mortality in this situation is a challenge that is extremely difficult to overcome. Attempts at estimating the incidence, morbidity and mortality due to snakebite on a global scale have typically floundered because of these problems.
GLOBAL ESTIMATES SINCE 1950
There have been three major attempts to produce global measurements of the snakebite problem since the 1950’s. While all of them have sought to use the best approaches available, each of them has been to a large extent incomplete or inaccurate to varying degree.
Author (Year) |
Snakebites |
Envenoming |
Deaths |
Swaroop & Grab (1954) |
500,000 |
- |
30,000-40,000 |
Chippaux (1998) |
5.4 million |
2,682,500 |
125,345 |
Kasturiratne et al (2008) |
1.2-5.5 million |
421,000-1,841,000 |
20,000-94,000 |
- READ MORE: Snakebite mortality in the world (Swaroop & Grab, 1954)
- READ MORE: Snakebite - appraisal of the global situation (Chippaux, 1998)
- READ MORE: Global burden of snakebite (Kasturiratne et al, 2008)
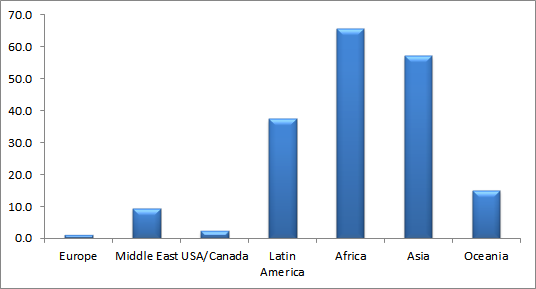
Regional comparisons of snakebite are also problematic, since the different parts of the world have vastly different public health systems, socio-economic bases, cultural and social values and infrastructure. The way in which data is presented also comes into play, when looking at the impact of snakebite. Dr Chippaux’s 1998 study reported the greatest number of envenomed patients (2 million cases) to be in Asia, compared to Africa (500,000 cases), but when this data is standardised to a population-equivalent basis, we can see, in the diagram below, that the rate of envenoming in Africa (65.8/100,000) is actually greater than that for Asia (57.1/100,000). Likewise 3,000 cases (15.0/100,000) of snakebite envenoming in Oceania is clearly a bigger burden on the overall population than the 6,500 cases (2.4/100,000) in the USA/Canada.
Overcoming the hurdle of obtaining good quality statistics is one that ultimately will require a narrower focus than a global lens. A number of good quality studies have been carried out within regions of countries by researchers who are on the ground and able to follow a predetermined data collection protocol. For example, in Nepal, Dr Sanjib Sharma and colleagues from the B. P. Koirala Institute of Health Sciences in Dharan working with colleagues from Switzerland was able to conduct a community based study of snakebite in 5 villages (Itahara; Kerabari; Chulachuli; Shivgunj; and Rajghat) across southeastern Nepal, knocking on more than 1,800 household’s doors at random and interviewing the occupants about whether anyone living there had experienced a snakebite in the previous 14 month period. The researcher identified 143 cases of snakebite, including 75 where envenoming occurred, and caused 20 deaths. These numbers enabled them to calculate, that for every 100,000 people in the region, there were 1,162 snakebites with 604 cases causing envenoming and 162 resulting in death. But perhaps most important of all, they were able to identify two important factors that contribute to fatal outcomes:
- Delayed hospital attendance due to first visiting a traditional healer; and,
- Absence of readily available transport to hospital.
- READ MORE: Snakebite impact in southeastern Nepal
Community-based surveys are extremely valuable, especially in communities where health-seeking behaviour might not necessarily put going to hospital at the top of the list of priorities. Poor rural farmers often cannot afford conventional medical treatment, or may belong to ethnic groups with strong ties to traditional medicine. In rural Cambodia, nearly all snakebite victims go to a traditional healer, before considering a trip to hospital, and the same if true for many communities right around the developing world. This is of course part of the reason why snakebite is often under-reported in hospital admissions data. Going direct to the communities to identify the victims of snakebite really is the best way to determine accurate incidence, morbidity and mortality figures for many places in Africa, Asia, New Guinea or parts of Latin America.
Hospital-based studies are an important source of information nevertheless. Dr Sharma and his colleagues in Nepal, also looked at over 4,000 cases of snakebite treated at 10 medical facilities in the eastern part of the country. Of these 379 (10.6%) had signs of snakebite envenoming, and there were 81 deaths (2%). They were able to build a profile of the seasonal pattern of snakebite, discover what the demographic profile of the victims was, determine at what time of day most of the venomous bites occurred, and calculate how much antivenom was being used. Taking a different approach, a team of researchers working in Thailand were able to collect and identify all of the dead snakes that victims brought to hospitals right across the country, and gain a much better understanding of what types of snakes caused snakebites in different areas. This sort of information can be invaluable in correctly treating snakebites, and in making sure that the right types of antivenom are held in the hospitals.
- READ MORE: Snakebite reappraisal in eastern Nepal
- READ MORE: Hospital survey of species causing snakebites
Establishing standard data collection approaches to documenting snakebite cases is an important step that needs to be taken if future estimates of the problem around the world are to be meaningful. The Global Snakebite Initiative’s Medical & Scientific Advisory Committee will be tasked with developing draft guidelines for standardising the collection of epidemiological and basic clinical data on snakebites, and creating standard research protocols and documentation that can be used to undertake such studies in a wide range of settings. By making these guidelines and protocols available freely, we hope to improve the quality and quantity of data, so that accurate estimations of snakebite burden can be carried out.